Developing caseload management skills in your early career (in Private Practice!)
There’s no doubt that managing a caseload effectively is a priority area of growth and development not only in your early career years, but also as your caseload complexity and client load increases throughout your professional life.
In our recent free workshop on Excellence, one of the key themes we explored was the polarity (seemingly opposing values) of Quality & Efficiency – in relation to a clinical caseload. Note, that the information below relates to working primarily in a Paediatric Private Practice setting, although some of the principles are definitely able to be extrapolated to other settings, simply run the information through your frameworks or procedures around service delivery.

Today in this blog we want to dive a little deeper, and elaborate on an area that was recently requested via email: Navigating an increased clinical load as a new grad – ensuring quality but working efficiently!
In July we will be hosting a webinar targeting this topic specifically, which will go further in depth into the following areas.
- Boundaries and valuing yourself
- Self-Organisation and forward planning
- Understanding direct/indirect services and not working for free
However, for today, let’s explore the final point:
There are two lens to look at caseload management through: direct & indirect services.
Given that each clinician will have strengths in different areas, as we move through the following questions – ask yourself, ‘what is the difference that will make the difference, for me?’
Managing caseload demands falls within two broad areas: The services we provide clients that are direct (face to face) services, and the work that we do that is indirect, or happens without the client in the therapy room. Both are important parts of clinical management, that require focus and intention from clinicians. As clinician’s progress in their professional skills, the focus can often expand from simply providing high quality direct services, to also valuing and delivering high quality indirect services to clients. The following questions/tips will potentially reveal barriers that may exist for clinicians, in developing both their skills and also their ability to communicate the value of both services.
Direct Services
Read research
It’s simple, but effective. Dedicating 30m a week to reading 1x research article related to an area of your practice is a pro-active skillset that will dramatically improve your capacity to understand & integrate clinical information across a variety of areas of practice. Improving clinical quality and efficiency is usually easily understood by clinicians as ‘knowing what to do with their clients’. Reading research articles to develop your clinical reasoning will help you in your assessment analysis, client communications, and ability to make modifications and adjustments with stakeholders across environments, as the implications of your clinical goals become more apparent.
Understand & communicate your current scope of practice
If you are working across a generalist caseload, how would you define this? What 8-10 areas of speech pathology practice are you confident & competent in administering? Have you communicated this to your workplace, and is there a plan in place for you to develop in the areas of practice you feel less sure about? Or clinical protocols for you to follow? If not – these unfamiliar areas will require additional time, effort and research in order to conduct your session planning, administration of assessment & goal setting. This should be prioritised in clinical supervision, and also kept to a manageable level with regards to your caseload diversity.
Know how many stories you are holding
Each family that we have the privilege of working with comes with their own ‘story’, which includes their background, stakeholders, communication requirements and general emotional complexities. In any ‘helping’ profession we understand that working directly with clients involves some ethical cross over, and without awareness of this it can lead to holding onto emotions that don’t belong to us. It’s worthwhile considering how many families are on your caseload, and factors here will include the length of appointment times (e.g. do you see 10 x 30 min appointments or 5 x 1 hour appointments in a 5 hour billed day), alongside therapeutic frequency (i.e. a fortnightly caseload will double the number of ‘stories’).
Some university degrees (e.g. UQ) cover the principles of transference & counter transference in their ethics lectures, and developing self awareness of your emotional boundaries, and learning to develop good self-responsibility around the emotional management of your caseload is important.
Indirect Services
Stop calling it ‘admin’
As clinicians, we often get requests for various aspects of clinical care that are required to be conducted outside of session times. It’s important to understand the elements involved in the type of care that is agreed to, and to determine what is appropriate to absorb as part of general clinical practice & what is specifically required as consultative support for the case.
For example, general clinical practice might include; session planning, resource gathering, scheduling.
Client Related Indirect Services might include; 
- Writing of letters, reports, summaries additional to existing documentation
- Attendance at meetings, including phone calls, zoom calls, or face to face meetings (including travel time).
- Development of clinical resources specific or individual to the child, as required for their intervention
- Provision of adjustments or classroom scaffolds, curriculum modifications/support and environmental recommendations/adjustments.
- Advocacy, education of stakeholders, case management advice, including lead therapist planning time.
- Multi disciplinary and interdisciplinary stakeholder in person communications, includes collaborative goal setting & clinical planning sessions, case conferencing & review meetings.
- Home programming, individualised resource development, AAC planning or programming.
- Parent advice, education, coaching sessions.
Clinical services such as those mentioned in the list above are clearly considered as directly related to an individual case, and should be scheduled and communicated as if they were appointments, if you are working as part of a fee for service model. This will both improve the efficiency & quality of clinical care, as well as reduce the overwhelm that clinicians can develop as a results of ‘admin building up’.
Understand & communicate your model of care
This is an area that will be specific to the workplace setting you are operating within, however simply to mention that different service delivery models will require different communication requirements. E.g. if you are working within a Speech Pathology specific practice, in a single-discipline model, the stakeholder communications & documentation will vary significantly from working within a multidisciplinary or interdisciplinary model, alongside multiple stakeholders, when providing collaborative or coordinated care. Typically the list of indirect services (above) is a good starting place to understand how the communication requirements might change, as the service delivery model becomes more complex. Factoring this additional complexity into your caseload planning & administrative time is important.
Get really good at using a scheduling app
If you are still using a ‘to do’ list – it’s time to upgrade your self-organisation. It was a few years ago that I (Marion) realised ‘planning’ didn’t exist. It’s easy to sit and stare at the diary, or to do list, and convince yourself you are being productive by ‘planning’ the week. It can be more useful however, to break down planning into a subset of skills – and then work on radically improving your capacity to execute each skill:
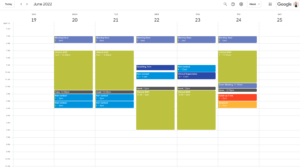 1. Create your Schedule – This means, understand your work-life boundaries, define your working hours, and your contact/non contact times. Understand what buckets of time you have to work with, and the breakdown of hours that lives inside each one. Consider also your travel time, outside of work commitments, and general weekly flow of energy (where/when do you feel good throughout the week). Using a calendar app like gCal is extremely effective at creating a visually-defined boundary for these times & the 10 min notification reminders are useful also to help you stick to it!
1. Create your Schedule – This means, understand your work-life boundaries, define your working hours, and your contact/non contact times. Understand what buckets of time you have to work with, and the breakdown of hours that lives inside each one. Consider also your travel time, outside of work commitments, and general weekly flow of energy (where/when do you feel good throughout the week). Using a calendar app like gCal is extremely effective at creating a visually-defined boundary for these times & the 10 min notification reminders are useful also to help you stick to it!
2. Prioritise – Now organise your list into categories, there is a variety of ways to do this. You can group tasks by content (e.g. reports, stakeholders to contact, letters to write, resources to develop), by time (5 min jobs, 10 min jobs, 15 min jobs, 30+ min jobs), or by need (e.g. google Eisenhower matrix – urgent/important ranking) or a combination. How you prioritise might change depending on what you have to do – however being able to prioritise based on what is actually most important right now is a skill requiring discernment, and reflection over time. What do you tend to say yes to, to which you should be saying not now?
3. Allocate & Communicate – Now you have both the time frames & also the priority order, so you can scan ahead the next 1-3 weeks and allocate the tasks into the buckets of time that you have available. Which tasks & when? As you map it out – how does that change what you need to communicate to clients, team members or supervisors about your capacity? Have a 15 min time block where you zoom in & out on this plan on a weekly, or bi-weekly basis, to reschedule & reprioritise based on new requests or information.
3. Execute – Now you have both the schedule set & priorities clear, and you’ve communicated that to the relevant people, it’s time to action. Notice here – any procrastination, distraction or mindset barriers that might arise in the moment & address these.
In summary, navigating an increased clinical load is a skillset that will continue to develop over many years of practice, however some of the practices above can dramatically reduce the experience of overwhelm, and burnout related to difficulties with accurately judging, planning & communicating the elements involved in excellent caseload management. Each clinician will find growth available in different aspects of caseload management, with some parts coming more easily than others, and growing and developing through your own unique areas of difficulty is part of the pleasure of self development and professional goal setting. Seeing areas of difficulty as opportunity for growth, and an exciting challenge to address is a useful mindset for the aspects of our clinical practice that feel most challenging.
At Cooee, all team members receive 1:1 Developmental Coaching, which is targeted around their own self-leadership. That is, their capacity to create change, or difference, for themselves, in their own professional lives. We use an Integral Framework to develop specific strategies and tools that target areas of growth unique to the skills that each person requires to grow, across four areas of mindset, culture & communication, action taking & developing systems.
This coaching is also offered external to professionals & clinicians working outside Cooee (by fee), and to express interest book a 1:1 coaching exploration call with Marion!
